I Nyoman Sutarsa
Accessing appropriate and quality HIV-related health services in a timely manner was never easy for Putri (a pseudonym), a male to female transgender 26 year-old who lived in West Bali. The relatively low prevalence and incidence of HIV in her district meant it was not considered a priority area for HIV prevention and treatment. As a transgender person Putri occupied an uneasy position in Balinese society, which follows a patriarchal structure where men gain more privileges than women. Putri’s families, relatives and many people around her blamed her for her choice. She was socially punished because she did not conform to societal expectations and for some people this act is simply assumed to be amoral.
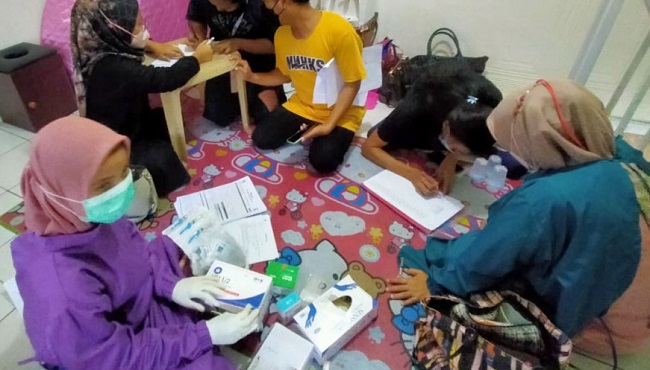
During fieldwork for my doctoral thesis in 2016, Putri was admitted to the district hospital due to shortness of breath and was diagnosed with lung tuberculosis. She was sent to the voluntary counselling and testing services where rapid HIV testing was performed and came back positive. This information spread fast. As is the case for all newly diagnosed HIV cases, because she was perceived as a threat to the community Putri was required to reveal her private sexual life to bureaucratic entities. She became an object of surveillance not only in the context of public health, but also as a target for moral surveillance. Putri encountered dual stigma and discrimination related to both her HIV status and her gender non-conforming identify. These dual stigmas did not operate in silos but interacted in complex ways to create disparities and social inequities.

At the time of my fieldwork in West Bali, the outreach program for transgender people received limited funding from the health office. If Putri had been living in Bali’s capital, Denpasar, where most support systems are available for transgender people, she would probably have had a better chance of being diagnosed earlier and could have started treatment sooner. She did not benefit from the joined-up service provision that is available in Denpasar. Since the early days of the HIV epidemic, Denpasar has been a priority area for HIV and AIDS programs, including community-based interventions for transgender people. The limited availability of outreach programs contributed to her late diagnosis.
Putri’s story illustrates the intricate relationships between morality and the notion of risk embedded in public health discourse. The rhetoric of moral pathology has influenced political decisions around the allocation of health resources, program implementation, target populations and ultimately, which groups of people are left behind. These decisions also act to inhibit some people from exercising their choice to access healthcare.
Inequities have consequences
Putri’s late diagnosis and premature death highlight how inequities in service availability affect access and use of HIV-related healthcare among transgender people. There were no tailored outreach activities or peer support programs that could assist Putri in navigating the complex HIV and AIDS care and service provision. She did not benefit from Indonesia’s comprehensive HIV program implementation in place for over two decades that included contributions from external donors, local non-government organisations and political commitment from the provincial government.
Her story reveals that inequities in access to essential health services are not random. Locating comprehensive HIV services within priority districts may save lives, and this decision is economically defensible. However, in doing so, it denies many people a fair chance at significant benefit and can lead to catastrophic consequences including premature deaths.
Timely access to quality health services is a basic human right. Regardless of their political affiliation, gender, sexuality, socio-economic positions, religious beliefs, and cultural background people should have access to essential health services when they need it. Achieving this right is a daily struggle for many ‘marginal’ populations. During the COVID-19 pandemic, around the world socially and economically disadvantaged individuals have been disproportionately affected, both mortality and morbidity. Such impacts, including the inequitable access to health care and an economic safety net, were further exacerbated by the interconnected structural risks - inequities in wealth, lack of social protection, unfair employment structure and maldistribution of health infrastructure and health resources. Such findings tell us that in order to address inequitable access to healthcare calls there needs to be a new framing of the problem that moves away from the level of the individual to analysis of social structures and norms.
Inequitable access to health care is a major determinant of lower health outcomes, including late diagnosis, high morbidity and even premature and preventable death. These effects are palpable, inequitably distributed and more pervasive in the everyday life of marginalised individuals, those who live in the intersection of poverty and social oppressions.
Intersections of disadvantage
Before we can take action to eliminate inequities related to access to healthcare, it is imperative to fully comprehend the root causes. Putri’s story, like so many heard during the COVID-19 pandemic, highlight the tragic consequences of such inequities for communities at the intersections of poverty and social exclusions. It exposes the longstanding structural causes: precarious working conditions and employment structures, inequitable distribution of income and wealth, growing economic disparities, living arrangements, and social isolation and fragmentation. These systemic risks are interrelated with class, gender, education and other oppression systems and during the pandemic, amplified existing social vulnerabilities in society.
To move forward in addressing access inequities, we need to recognise multiple oppression systems and privileges at various levels. Access inequities are shaped by different factors and social dynamics operating simultaneously, where people can experience privilege and oppression at the same time depending on specific contexts. Actions to redress access and health inequities must be reoriented to reflect this intersectionality that links individual lived experiences and broader structural factors. For example, representing transgender people as having similar needs to those of the general population leads to a failure to understand the unique health needs and structural oppression they experience. Similarly, treating the whole transgender population as a single group is insufficient because it ignores the intragroup diversity that offers lessons for policy formulation, program design and service delivery models.
New approach
Addressing inequitable access to healthcare requires health practitioners to disentangle the intersecting systemic risks to effectively redress health inequities. By applying an intersectional analysis, connections between individual attributes, institutional arrangements and structural determinants in a given sociohistorical context can be explicated. Such insights are important in any attempt to address social inequity and to promote social justice. An intersectional analysis provides practical benefits to health system processes, for example: in carefully designing the target population, in recognising which populations should be protected by public health systems, or in identifying what interventions should be promoted. It can also guide meaningful impact monitoring and evaluation of any social policies and programs on different subpopulations, from the most disadvantaged through to the most privileged groups.
Programs and interventions that target the general population through mainstreaming HIV services into community health centres are failing to address the fact that those on the margins miss out. Health bureaucrats assume that predisposed and need variables are equitably distributed across different groups. In fact, these risks are not evenly distributed. They are shaped by diverse structural and social determinants including gender, class, morality, social norms, religious values, and political and economic forces. Such narrow assumptions can conceal differentiated risks resulting from the unique social position and conditions of marginalised groups.
For HIV services to be accessible by transgender people, those services must attend to the interconnected structural determinants that influence people’s access to adequate economic opportunities, appropriate health and social care, and quality and friendly health services.
I Nyoman Sutarsa is a lecturer at the Australian National University Medical School and Department of Public Health and Preventive Medicine, Faculty of Medicine, Udayana University, Denpasar.



