Special Autonomy has crippled health services in the Papuan Highlands
Bobby Anderson
The entrance of a closed district health centre in Bokondini, Tolikara. The medicines destined for this centre were re-sold in Wamena. Residents rely upon medical supplies in the privately-run Ob Anggen school. Bobby Anderson
Under Papua’s Special Autonomy Law the majority of Papua’s natural resource wealth is returned to the province. This 2001 law was meant to address both the sources of political unrest in Papua, and the challenges ordinary Papuans experience on a daily basis. It was meant to increase Papuan access to government jobs and economic opportunities, as well as to health and education services. A dozen years and billions of dollars later, most Papuans still live in misery. Papuans have the highest malnutrition, tuberculosis and HIV rates in Indonesia; as well as the lowest incomes and the highest mortality.
Special autonomy has failed. But the greatest failure has little to do with the aspects of special autonomy that were poorly implemented by Jakarta. The greatest failure, for ordinary people, has to do with those aspects of special autonomy that were handed over to provincial and district officials: health and education services.
In a previous article, ‘The failure of education in Papua’s highlands’, I described how local officials and elites no longer see special autonomy as a means to development. Rather, they see it as a way to access greater national subsidies, which they can take for themselves or spread through their patronage networks in the form of jobs or other benefits. I also described how the failings of special autonomy are enhanced by the uncontrolled creation of new districts, sub-districts and villages under the process known as ‘pemekaran’ (proliferation), which allows local clan elites to access funds while pushing ordinary Papuans further away from the services that could improve their lives.
The interplay of these policies has destroyed the education system in the highlands. In this article, I will discuss how and why this process has been equally destructive to health services.
The end of an already-struggling system
In Papua’s highlands, the marriage of special autonomy funding with elite political and clan machinations has combined to break the healthcare system.
As with education services, healthcare in the highlands was initially provided by local churches and missionaries. The Dutch government – and later the Indonesian– recognised the churches and kept them in place as service providers working on behalf of the state. In this model health centres were staffed and functional, and midwifery services, immunisation programs, and mother and child health programs were accessible. District health departments paid health workers on site, and in Jayawijaya and a few other areas, there were local health insurance schemes.
Even at their best, however, these services provided healthcare to the minority of highlanders who were able to access such services. Most highlanders lived in remote areas and remained without health services. The fragmentation of this system, which I described in greater detail in 'Living without a state', 'The failure of education' and other articles, occurred when the state took over these services at the end of the Suharto dictatorship.
After the takeover, these systems were no longer managed locally. Instead, new government administrators based in district capitals were remotely running systems in places they had never visited, coordinating employees they had never met. The system was further shaken by the 2001 riots in Wamena, when Papuan rioters killed dozens of Indonesian migrants. These killings created a reverse migration flow as migrants – many of them healthcare workers – left to the cities. Replacement healthcare workers were hired not according to their skills, but according to their clans and, in most cases, they were not expected to show up for work.
The uncontrolled creation of new administrative structures destroyed already weak healthcare systems in newly created administrative units, and to the present day such systems have yet to be rebuilt. With the exception of Wamena and a few other areas, healthcare services essentially disappeared. Virtually everything stopped; from classes for new mothers and infant immunisations, to the provision of tuberculosis and malaria drugs. The end of this system in many remote areas coincided with the arrival of HIV/AIDS.
The state of healthcare in the highlands today
A few communities are able to benefit from the remaining services provided by private foundations, community-based organisations, or churches. There are also still a few functioning government-run community health centres in the sub-district capitals, village maternity posts and community health outreach services in the villages. But access to services is mostly an urban story. District capitals have erratic, but functioning, services. In newly created administrative districts these services are only now beginning in their capitals, though Special Autonomy became the policy in 2001. In the majority of rural highland areas there is simply nothing available. A few notable non-state actors provide services in rural areas where they can: the local non-government organisation (NGO) Yasumat provides parallel health services in half of the sub-districts in Yahukimo. In areas of the highlands accessible by road from Wamena, erratic state-provided services are accessible via occasional public transport to functioning areas.
The rugged topography of the highlands is used as a blanket excuse for this lack of health services. That an earlier, church-run system once existed during an era of even less infrastructure and funding has been forgotten. But this ruggedness does provide real barriers: according to the World Bank’s 2006 Indonesia Poverty Analysis Program, an average Papuan household lives 32 kilometres from the nearest health clinic, while in Java, the distance is only four kilometres. These distances increase the further one moves inland from the coast, in the mountains this means days of walking on steep paths to access healthcare.
 A medical centre run by volunteers in Bonohaik, Lolat, Yahukimo. Bobby Anderson
A medical centre run by volunteers in Bonohaik, Lolat, Yahukimo. Bobby Anderson
The deep causes of health service delivery failure are not found in geology or plate tectonics, however. They are found in clan politics and flawed human resource management: decentralisation concentrates decision-making power over the provision of services at the district level, where district heads often act like feudal lords distributing favours and jobs. And the creation of administrative districts allows for more and more local elites to create their own districts and so access funding streams. A pantomime occurs to mask these motivations, one in which the creation of administrative districts is depicted as needed to bring services closer to an under-serviced populace. This is a lie. In new decentralised health care systems, services stop.
In ‘Land of ghosts’ I illustrated the excuses that health department bureaucrats give to explain why they cannot do their jobs, and which result in patients being refused care. Staff at health centres located in districts out of which new administrative districts have been formed will direct residents of the new districts’ health centres, even where such centres do not yet exist.
The same goes for sub-districts, which proliferate at a seemingly viral rate. Many sub-districts created a decade ago still do not have the functioning health system every sub-district in Indonesia is supposed to have. In most of these places the new administrative centre has been built, but construction is only the beginning. Many centres remain closed because, for example, no head has been appointed. Or the head has been appointed, but no accommodation has been constructed. Or the accommodation has been constructed, but it is sub-standard. Or the centre has been constructed and the head has been relocated, but there is no equipment. Or none of the other staff have arrived. Or they refuse to relocate because there is no functioning school nearby for their children. Or perhaps, staff have been appointed and come to the centre, but because they get paid only in the district capital, they have to travel there often and are not on hand to provide services to patients most of the time.
In the meantime, the only services available are in the original health centres in the old sub-district centre, whose annual budget, calculated on the basis of the sub-district population, was reduced when a new sub-district was created. And so decentralisation results in the same administrative system serving the same people but with a drastically reduced budget. Many centres refuse service to ex-residents who reside in new sub-districts because of this income loss. And, it goes without saying; the funding that was lost because in reallocation to the new sub-district is often ‘mislaid’.
Staffing is the key
One might assume that existing health centres in areas not yet decentralised function well. This is also false. All of the excuses to explain why teachers and other civil servants are absent from their remote posts are also used by absentee healthcare workers. These excuses have been repeated for years and have never been addressed by district authorities that have the power, and the funding, to do so.
The reason why staffing problems are never resolved is that the people who are hired for these jobs might have the appropriate clan and political affiliations, but they lack the appropriate skills (they may be products of the failed highland educational system) and are not expected to show up for work anyway. District leaders often dictate hiring practices to award their own clans and allied clans that supported their last election campaign. Jobs in this context are just another asset to be distributed among the clan or to reward political supporters. That’s the basic problem: proliferation of new administrative units and the creation of new government offices often have nothing to do with the provision of services, despite all the talk to that effect.
A minority of the administrators and healthcare workers in this system actually do try to do their jobs, but their performance is hobbled by the majority. For lower-level workers in certain districts, so much of their salary is siphoned off before they receive it that they no longer have a wage they can live on. The head of district health services in Tolikara lamented in 2011 that a high turnover of administrators was the cause of inadequate health services in her area. However, the last administrator was driven out by her when he tried to pay health workers directly, instead of paying though her and allowing her to skim off a 50 per cent gratuity on each salary paid.
And yet, as in education, the problem of health service delivery is assumed to be an infrastructural one, and so new district, sub-district, and village health centres are built with special autonomy funds. It is as if a profusion of qualified and eager workers exist in these areas but they simply lack the roofs and the tools to treat people. In fact, the opposite is true. Sub-district capitals usually have health centres equipped with beds, cabinets, baby-weighing scales, and other equipment. In at least some villages, smaller health centres do exist. The buildings are standing, but they are locked: health staff have never been present. I have treated wounds in Ninia and other areas with my own first aid kit, a stone’s throw from locked health facilities. The few health posts that are regularly open are overwhelmed: people walk for days to access them.
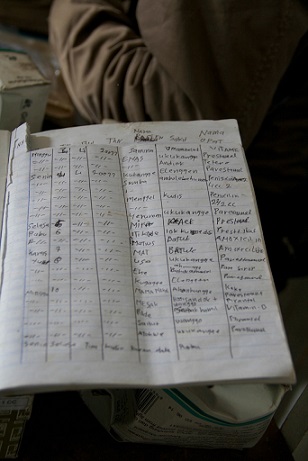
 The patient guestbook in Bonohaik, listing medicines dispensed. This is one of the best-run volunteer clinics I’ve seen in the highlands. Ita Perwira
The patient guestbook in Bonohaik, listing medicines dispensed. This is one of the best-run volunteer clinics I’ve seen in the highlands. Ita Perwira
This system occasionally struggles to life, and manifests itself in a new set of HIV awareness posters or an unscheduled medicine delivery to a village health centre. But medicine provided to villages is not accompanied by instructions, and it is often expired. This year I have taken inventory of such stocks in village health centres in Yahukimo, Tolikara, and Memberamo Tengah, and have found medicine that expired in 2007. That same medicine was delivered in 2011. Unexpired medicines are often destroyed due to improper storage – when the village health centre is locked, the medicines often end up in boxes in the corner of a church. With no health workers present, ailing villagers are often reduced to picking through these stocks in a vain attempt to self-prescribe, popping pills from containers with unreadable, waterlogged labels.
The health of Papuans
This absence of health services occurs in a province that has the lowest life expectancy in Indonesia. The life expectancy of indigenous Papuans is significantly lower than that of the migrant population, which is close to the national average. Migrants are concentrated in towns, where health services still function. Indigenous Papuans are concentrated in rural areas, where they do not.
The most significant health issues facing indigenous Papuans are not the ones that national and international media concentrate on. HIV/AIDS is a serious issue, but it is not the most significant public health threat it is made out to be. Statistics on Papua should be used and referenced with great caution, and this is doubly true of the highlands. However, the numbers that are available in select studies rank Papua last in every human development indicator.
Let’s begin with the young: indigenous Papuans have the highest infant, child, and maternal mortality rates in the country. The 2012 Indonesia Demographic and Health Survey Preliminary Report prepared by the Ministry of Health, the National Population and Family Planning Board, and other agencies indicate that, in Papua, 40 per cent of babies were delivered by a skilled provider: in Jakarta, the rate was 99 per cent. In Papua, 27 per cent of babies were delivered in a health facility; in Jakarta, the rate was 96 per cent.
The report paints a vividly negative picture of child mortality rates in both Papua and West Papua provinces, especially in comparison to Jakarta. In Jakarta, 22 babies out of 1000 die, but in Papua this number increases to 54, while in West Papua, the number increases to 74. In Jakarta, only 31 children under five out of 1000 die, but in West Papua this number increases to 109, and in Papua it increases to 115.
The Health Survey report indicates higher neonatal (1-30 days), post-neonatal (30 days to one year), and infant (over one year) mortality rates in West Papua province than Papua, which is unusual, considering that West Papua’s health services are nowhere near as problematic as Papua’s. I believe that the report is unrealistically positive with regard to Papua. Myself and others who have spent time in remote areas of Papua and West Papua ascribe the latter province’s more negative showings in neonatal, post-neonatal and infant mortality to a mistake in numbers the researchers had access to in order to undertake their correlations on mortality. It’s not that Papua actually has lower mortality rates in these categories. It’s that West Papua is better at counting its dead.
These figures are also skewed in that they include the most populous cities and the most remote hamlets. A baby born in Jayapura and a baby born in Sinokla do not have the same likelihood of surviving their fifth birthday: the difference is so great that they might as well be born on different continents.
The death rate worsens in the remote areas for which statistics are available. The French NGO Medecins du Monde worked until recently in Puncak Jaya, one of the most remote areas of the highlands, and the only one with an active OPM (Free Papua Organisation) presence. In 2008 they estimated an infant mortality rate of between 85 and 150 per 1000 live births in the district. As for how these infants and children die; the most common cause is acute respiratory infections (especially pneumonia), followed by diarrhea and malaria. These killers are so common in rural communities that they are considered normal.
The major underlying cause of these deaths is malnutrition: in the highlands and remote lowlands, it is visible in every group of children, in their bloated stomachs and spindly limbs. The mothers who die in childbirth usually succumb to blood loss or neonatal sepsis, and malnutrition indirectly contributes to this as well, especially through anemia and weakened immune systems.
The provincial prevalence of malnutrition (as measured by weight and by age) of 21.2 per cent is higher than the national rate of 18.4 per cent. In the highlands, this prevalence may be as high as 40 per cent. Malnutrition is not simply ‘hunger’. For children, it weakens the immune system, stunts physical growth, and inhibits mental and cognitive development.
Parasites are one common cause of malnutrition: children must compete for a finite amount of nutrients with the worms in their bodies. All of these conditions are further exacerbated by the lack of access to clean water, lack of hygiene, and inadequate sanitation. The foundation of these negative conditions and practices is a lack of knowledge, a result of the disintegration of the health and education infrastructure over recent years.
Some malnutrition in the highlands is not caused by a lack of food per se: rather, it’s caused by the kind of food that is provided to children. Breastfeeding often ends too early in an infant’s life, and supplemental feeding begins too early. Mothers begin to feed their babies sago mash when the children are weeks old, and this is inherently harmful. The Jayapura Health Polytechnic’s Department of Nutrition (Poltekkes Gizi) undertook a study of feeding practices in Jayapura district in 2012. The study revealed that the poorest families had the healthiest babies, because those families could not afford supplementary food and had to rely on exclusive breastfeeding. This positive trend, however, reverses itself after about six months, as soon as supplementary food is needed.
 Medical waste disposal, Bonohaik, Lolat, Yahukimo. When it dries, it’s burned. This is better than other areas, where medical waste is dumped in piles, often to be consumed by pigs. Bobby Anderson
Medical waste disposal, Bonohaik, Lolat, Yahukimo. When it dries, it’s burned. This is better than other areas, where medical waste is dumped in piles, often to be consumed by pigs. Bobby Anderson
Care of expectant mothers, monitoring of pregnancies and infant health and weight, immunisation, and teaching and learning activities, used to occur through mother and child health posts which were once found in every village in Papua. When immunisation and other services ended, measles returned. Polio vaccinations also ended and now province-wide less than 50 per cent of children receive such vaccinations. In the highlands, the majority of children do not. In many new districts, no vaccinations have occurred since the creation of the district. Immunisations ended in the new district of Yahukimo in 2002 within months of the district’s formation, when the cold storage vaccination chain broke down. Vaccines become useless at room temperature. Suspected polio cases are now reported there, in Sumo and other extremely remote areas.
The tuberculosis epidemic
Tuberculosis (TB) is more of a public health threat than HIV/AIDS: it spreads via aerosol sputum, and can be transmitted, not just by sneezing and coughing, but also by speaking. Those living or working in close proximity to a sufferer will have an average 22 per cent infection rate. But TB health programs are drastically under-funded in comparison to those dealing with HIV/AIDS. Papuans have the highest tuberculosis infection rates in the country. Health foundations working in Wamena estimate a 10 per cent infection rate in Wamena town. In the rest of the highlands, it may be higher still.
Kalvari, a private clinic in Wamena, is widely recognised as the premier TB testing and treatment center: every district health department in the highlands refers patients there, and patients from Lanny Jaya, Tolikara, Mamberamo Tengah, Yahukimo, Nduga, and Yalimo travel for days to get there. Kalvari began testing TB patients at their clinic and found that nearly 50 per cent were HIV-positive: co-infections are common because HIV-weakened immune systems are easily infected.
The lack of healthcare services in the highlands has greatly contributed to this epidemic. TB is diagnosed via sputum smear microscopy, and only Kalvari and a few other highland service providers have the ability to conduct such tests, making the availability of diagnosis very limited. But the quality and accuracy of TB detection in any health centre is affected by error rates, which are in turn affected by the quality of testing equipment like microscopes and reagents. Even highly trained staff may have error rates of 25 per cent. Treatment itself is extensive and requires monitoring: medicines need to be taken for up to a year.
Kalvari’s treatment protocols for TB patients show the impossibility of providing trans-highland treatment through non-performing district health departments. Kalvari patients are asked to stay in Wamena for an initial two months of continuous treatment, and the group maintains a clean hostel for patients who have no family to stay with in Wamena. After two months, and another sputum check, patients who still test positive continue on-site treatment for another month. This is followed by another check: if patients still test positive, they are referred to a hospital for more intensive treatment. Kalvari’s small scale limits its ability to treat any more than a distinct minority of TB sufferers in such a comprehensive fashion.
Those patients who test negative after the initial two-month treatment move on to the next phase: they return home with a month’s supply of medicine. For patients outside Jayawijaya district, Kalvari refers their next treatment and sputum check to a functioning district health centre in their area. However, even with a two-month head start and comprehensive teaching by Kalvari staff of patients about the importance of finishing the treatment, the treatment drop-off rate is between 15 and 45 per cent.
Reasons for discontinuing treatment vary. In many cases, after receiving treatment for a few months, patients feel healthier and, without surveillance systems in place, stop treatment. Treatment side effects also lead to drop-off: bone pain and red-tinged urine are common. But the biggest cause of discontinuation relates to the supply of TB drugs: all too often, district health facilities run out of such medicines, or they only issue a few days’ supply of medicine at a time.
Some NGOs have attempted community monitoring programs, but the most important aspect of treatment – the drug supply – is too fractured for these initiatives to have any rate of success. And there is another, darker cause for the lack of TB drugs in some areas: it is mandated that these drugs be provided free of charge. The drugs in this form have no value to some profit-minded healthcare workers who instead sell them to private pharmacies that then charge patients.
Cases of multi-drug-resistant (MDR) TB become more frequent with every discontinued treatment cycle. Indonesia nationally is barely able to handle MDR cases: the country only began to address the issue in 2009, and has since opened ten MDR TB centres. In Jayapura, 20 cases have been detected, of whom 11 have already died. The greatest danger occurs when enough MDR patients fail to complete further treatment cycles, leading to extensively drug-resistant (XDR) TB, and then totally drug-resistant TB. The only protocol for the former, which kills a majority of patients, is years of treatment. The only treatment for the latter is isolation until death. The emergence of XDR TB in the highlands is not a remote possibility.
HIV/AIDS
Indigenous Papuans have the highest HIV/AIDS rates in the country, and Papua has one of the fastest-growing HIV infection rates in Asia. According to the United Nations Development Program (UNDP), 2.4 per cent of the Papuan population is HIV positive whereas the national average is 0.2 per cent. Migrants in Papua suffer HIV/AIDS rates at a percentage closer to the national average. The high percentage of infected persons is found within the indigenous population.
 A development worker taking inventory with two YASUMAT volunteers in a medicine dispensary in the corner of a church outside of Lolat, Yahukimo. Bobby Anderson
A development worker taking inventory with two YASUMAT volunteers in a medicine dispensary in the corner of a church outside of Lolat, Yahukimo. Bobby Anderson
In 2007 the Australian development agency, AusAID, predicted that by 2025, HIV rates in Papua would rise to seven per cent, compared to a nationwide infection rate of 1.08 per cent. However, health care workers in Wamena already estimate a prevalence of between eight and ten per cent in their region. HIV rates in remote areas of the highlands are unknown, but the number of young men, women, and children dying of unknown causes is out of proportion to the already abysmal provincial averages; a likely link to HIV’s spread.
Men working in the cities as part of the construction boom caused by the proliferation of new districts as well as an overabundance of special autonomy funding going toward infrastructure are contracting HIV from prostitutes. Wamena, Timika and other towns act as transmission areas for this and other sexually transmitted diseases. Ministry of Health Surveillance data (IBBS collected in May 2011) shows that 25 per cent of Wamena sex workers were HIV positive, while 35.4 per cent were infected with gonorrhea, 31.4 per cent had syphilis and 44.8 per cent had chlamydia. The majority of sexual transactions involving sex workers are unprotected, with the unhelpful exception of a local remedy: men cutting themselves to drain ‘bad blood’ after a visit with a prostitute.
The provision of prostitutes as ‘favours’ in local governmental patronage networks is now a standard practice and may help explain anecdotal evidence suggesting that the male Papuans who are contracting HIV the fastest are civil servants: village heads, election commission members, and so on. In Yahukimo’s Ninia sub-district, the district head’s home village, Balingama/ Yabi, has the highest rate of HIV thus far identified by one local NGO.
Another factor lending itself to increased transmission rates are local rural cultures that accept rape as a prerogative of ‘strong’ men: in a recent survey taken by a church foundation in Tolikara, a majority of young women revealed that their first sexual encounters were forced.
Many men who work outside their village bring their diseases home with them. Due to the absence of a healthcare system in these places, the worst impacts are realised. For instance, the prevalence of STIs may help explain increasing infertility of highland men and women, which is being noted with growing alarm by health NGOs.
For those who actually seek treatment for HIV through anti-retroviral (ARV) therapy, the availability of such drugs is precarious, even in Jakarta. In Papua, it is not possible to maintain a supply of ARVs unless one is rich. While in many parts of the world HIV is a manageable disease, in Papua – and especially in the highlands – it remains a death sentence for most people. For more see Carole Reckinger and Antoine Lemaire’s photo essay about people with HIV in Papua.
Anecdotal evidence indicates that most Papuans who die of AIDS-related illnesses were unaware that they had the disease. Nor did their families know. In villages across the highlands I have heard case after case of young husbands and wives dying of unknown wasting illnesses, followed by their children.
For those Papuans who are diagnosed, the notion of secrecy in testing does not exist: their HIV positive status may be revealed to their communities, and they rightly fear stigmatisation, with communities as well as immediate families often shunning HIV-positive people. Local churches preach that HIV is God’s punishment of sin. Spiritual mediums, drawing on beliefs that pre-date Christianity, teach that HIV/AIDS is a result, not of behaviour, but of curses, and that it can be cured through countervailing spiritual measures.
Fixing the system
The steps required to fix this dysfunctional healthcare system are by and large the same steps required to fix the education system in the highlands. First, relevant parties need to acknowledge the reasons why the system is broken. What is needed is healthcare workers who are present in their posts, as well as district administrators who actually manage health services. Medicines need to be available for long-term treatments. This means establishing supply chains, proper storage, and temperature maintenance (generally referred to as the cold chain), with trained personnel present across these steps.
Temperature maintenance is paramount: without it, the medicines are worthless. In fact, they can be worse than useless: attempts to treat TB with drug regimens that cannot be completed due to gaps in the cold chain foster MDR and XDR strains that will be harder, if not impossible, to treat.
 A patient awaiting treatment in Bonohaik. This man walked for days to seek treatment for his injured hand. He is days away from sepsis. Bobby Anderson
A patient awaiting treatment in Bonohaik. This man walked for days to seek treatment for his injured hand. He is days away from sepsis. Bobby Anderson
Workers who are not present, or are not qualified, need to be fired. In the feudalistic structure we call ‘decentralisation’, district heads are all-powerful, but they need to be divested of the right to influence human resources in district health services. It’s one thing to award no-show jobs in the civilian bureaucracy, where the salaries of such people simply suck funds from the system, but no-show healthcare workers result in unnecessary suffering and death. Such positions should be considered off-limits in local patronage games.
Medical workers need to be paid on site and provided with the support they need. Additional support for healthcare workers in remote areas should only go to new healthcare workers or those who have a record of attending their clinics. Providing absentee workers with additional support in the hope that they will work would be tantamount to rewarding people for their neglect.
In an interim period of repair of the state system, one option for provincial and district authorities would be to formally recognise the parallel institutions that were created to address the healthcare gap. These community-based service providers – Yasumat, Kalvari, and others – are already acknowledged as a critical part of the system. The workers could be put on the government payroll, but paid through the churches and other private institutions that run the systems.
Even making these changes would be cosmetic. The rot would remain, because it’s not simply healthcare and education positions that are given away as no-show jobs. There is not a single element of the bureaucracy in Papua that is not affected by this malaise. Special Autonomy has not worked. But its failure is disguised by a simplified discourse about Papuan rights that does not actually seek to fix what is broken within the system. Affirmative action has been reinterpreted as a person’s individual return on Papua’s natural wealth. The beneficiaries are local elites and those connected to them through clan or other ties. Ordinary people have been cheated out of meaningful education and healthy lives because of this.
Crushed by the wheels of modernity?
I am left with the image of a diminutive young Papuan man squatting on a flattened cardboard box amidst piles of trash discarded by migrant shopkeepers. I walked by that man one late evening in Jayapura in September 2011, and stopped to talk to him. In Jayapura for the first time, he spoke minimal Bahasa Indonesia. He’d walked from rural Keerom, a day or so away. He hugged his knees, his bags stacked against him. His rural skills and expertise were rendered obsolete in a paved and circuitboarded world far removed from his own.
This has been the fate of culture after culture as a relentless modernity bleeds into every corner of the world. The penetration of modern economies and the cultural changes that come with them cannot be stopped. But their effects can be ameliorated through the provision of knowledge and tools to the members of the cultures that are inundated. Only so equipped will they be able to defend themselves in this new world, and make their own decisions about how to adapt, no matter how hard those decisions may be. Education and health are critical to such self-defense.
While Papuans need education and healthcare, they are being fed with utopian fantasies about an inevitable independence that will cure all their ills. But if rural Papuans do not have access to functioning schools and health centres, they will be destroyed within a few generations. The continuation of the existing fragmented and dysfunctional system will result in an illiterate rural Papuan population with negative population growth rates, working at subsistence trades until they die prematurely. Every single person who takes a salary without showing up to work in the highlands health or education system is complicit in what ultimately may prove to be an autogenocide. To be bystanders in this continuing tragedy is also to be complicit in it.
This is a matter of urgency.
Bobby Anderson (rubashov@yahoo.com) works on health, education, and governance projects in Eastern Indonesia, and he travels frequently in Papua province. This and other articles on Indonesia can be found at http://independent.academia.edu/BobbyAnderson/.



